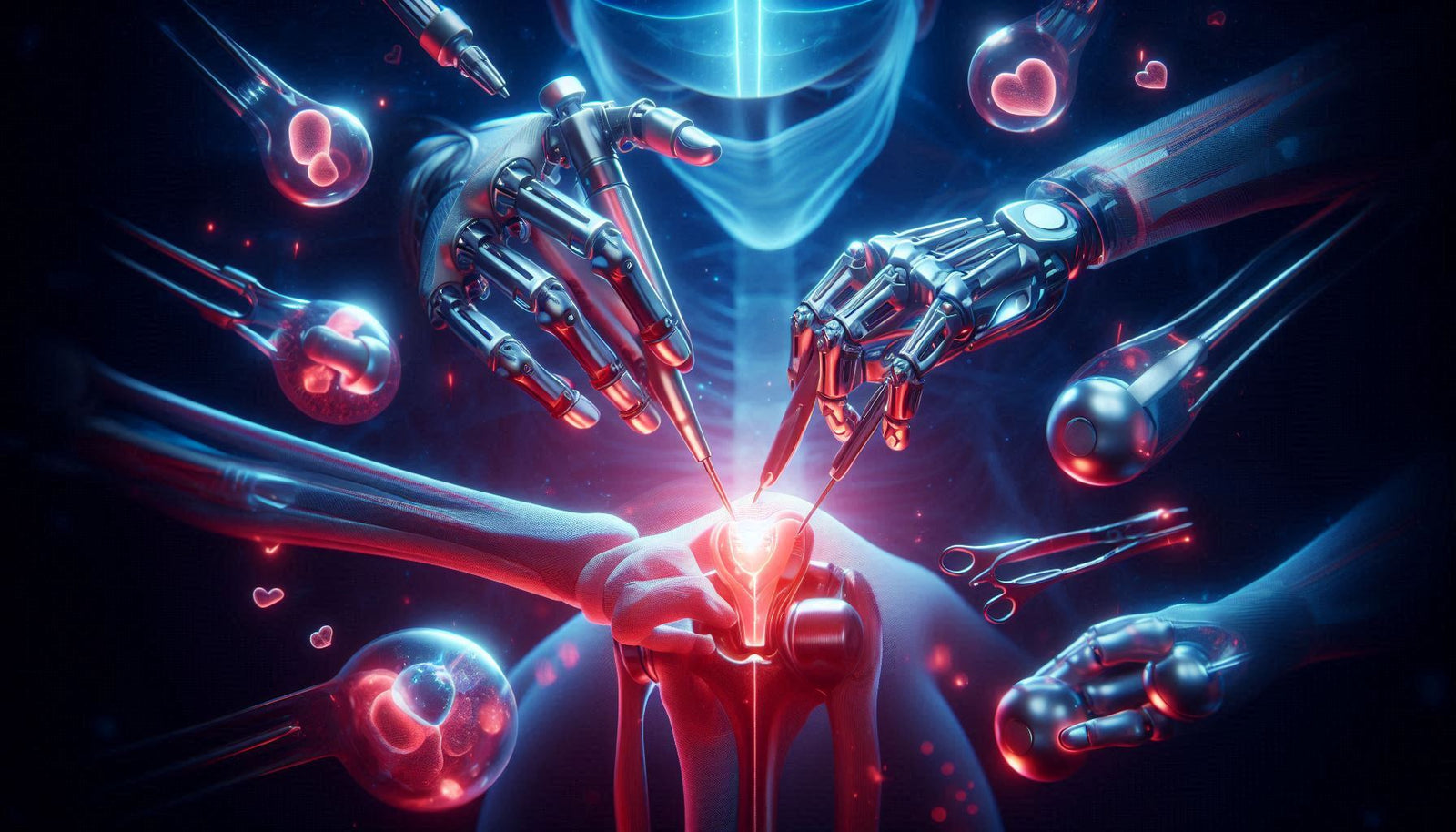
Orthopedic surgery has seen groundbreaking changes in recent years, with robotic-assisted joint replacement procedures becoming increasingly popular. From total knee arthroplasties to hip resurfacing, surgical robotics has ushered in a new era of precision, customization, and patient-centric care. This blog post explores how robotic-assisted surgery is reshaping orthopedic procedures, offering insights into the technology, benefits, real-world applications, and future possibilities.
What Is Robotic-Assisted Joint Replacement?
Robotic-assisted joint replacement surgery involves the use of robotic systems to guide surgical instruments with pinpoint accuracy. Unlike autonomous robots, these systems are controlled by trained surgeons who leverage detailed 3D models of the patient's anatomy for more precise implant placement and alignment. A well-known platform used in this space is the Mako Robotic-Arm Assisted Surgery System, developed by Stryker.
The system typically works in three phases: pre-operative planning, intra-operative guidance, and post-operative analysis. First, a CT scan of the patient's joint is used to build a personalized 3D model. This allows the surgeon to plan the surgery in advance, choosing the optimal implant size and position. During surgery, the robotic arm assists the surgeon by ensuring movements stay within the pre-defined boundaries, reducing the risk of soft tissue damage.
Why the Shift Toward Robotic Systems?
Traditionally, joint replacements relied heavily on the surgeon’s experience and mechanical instruments to determine alignment and implant positioning. While effective, these techniques can result in inconsistencies, especially for complex cases. Robotic systems, by contrast, bring several enhancements:
- Greater accuracy: Better alignment and implant positioning reduces the risk of revision surgeries.
- Personalization: Customized surgical plans using 3D imaging.
- Consistency: Lower variability in outcomes across patient populations.
- Reduced trauma: Smaller incisions, less disruption to surrounding tissues.
- Improved recovery: Less pain and faster rehabilitation.

How It Works: Step-by-Step Overview
- Imaging: A CT scan captures a detailed image of the joint.
- 3D Modeling: Software creates a virtual model used for planning the procedure.
- Pre-Planning: The surgeon selects the optimal implant size, orientation, and alignment.
- Surgical Execution: The robotic system guides the surgeon’s instruments to match the plan precisely.
- Verification: Real-time feedback ensures all steps are completed within tolerances.
Current Applications
While initially applied to total knee replacements, robotic-assisted systems are now used for:
- Total Hip Arthroplasty (THA)
- Partial Knee Replacement (PKR)
- Hip Resurfacing
- Spine surgeries (emerging)
- Shoulder replacements (in limited centers)
Clinical Outcomes and Studies
Studies published in peer-reviewed journals show that robotic-assisted procedures consistently result in:
- Improved implant alignment and positioning
- Reduced post-operative pain
- Faster return to activity
- Lower complication rates
- Fewer revision surgeries over time
For example, a 2023 study in The Journal of Arthroplasty reported a 35% improvement in implant alignment accuracy for robotic-assisted total knee arthroplasties compared to manual techniques. (Source)
Challenges and Limitations
Despite its advantages, robotic-assisted surgery is not without drawbacks:
- High initial cost: Robotic systems can cost upwards of $1 million, excluding training and maintenance.
- Training requirements: Surgeons and staff need specialized training and certification.
- Access disparities: Not all hospitals—especially rural or smaller facilities—can afford these systems.
- Insurance coverage: Some insurers do not cover the additional cost unless proven more effective. (Source)
Patient Experience and Recovery
Patients often report a more positive post-operative experience, including:
- Less post-surgical pain and reduced use of opioids
- Shorter hospital stays (often same-day discharge)
- Improved range of motion and joint stability
- Quicker return to work and daily activities
Patient education is key. Understanding what robotic-assisted surgery involves—its benefits, risks, and alternatives—can empower better decision-making and realistic recovery expectations.
Who Is a Good Candidate?
Not every patient qualifies for robotic-assisted joint replacement. Good candidates typically:
- Have localized joint arthritis without severe deformity
- Have sufficient bone quality and healthy surrounding tissues
- Are medically stable for surgery
Patients with multiple comorbidities, extensive bone loss, or complex joint deformities may not benefit significantly from robotic assistance—or may require more advanced customization.
Future Trends in Robotic Orthopedics
The next frontier includes:
- Integration with artificial intelligence (AI): Algorithms that optimize surgical planning in real time.
- Remote telesurgery: Performing procedures across distances using robotics and 5G. (Source)
- AR/VR integration: Augmented reality for enhanced visualization during procedures.
- Personalized implants: 3D-printed patient-specific prostheses based on robotic planning.
As this technology continues to evolve, we may see even more minimally invasive procedures that result in less trauma and better outcomes.
Advice for Providers
If you’re a provider considering robotic-assisted systems:
- Assess the ROI carefully: Consider volume, payer mix, and regional demand.
- Invest in team training: Include not just surgeons, but also anesthetists and nurses.
- Educate patients early: Use multimedia tools to explain the technology and set expectations.
Advice for Patients
Before committing to robotic-assisted joint replacement, ask your surgeon:
- How many robotic-assisted procedures have you performed?
- What are my non-robotic alternatives?
- What is my expected recovery timeline?
- Will my insurance cover the robotic portion of the procedure?
Conclusion
Robotic-assisted joint replacement represents a significant leap forward in orthopedic surgery. While not without its limitations, the technology offers improved outcomes, enhanced precision, and better patient satisfaction in many cases. As costs decline and training expands, robotic systems are likely to become the standard of care for many orthopedic procedures.
Whether you're a patient exploring treatment options or a provider considering a technology upgrade, robotic-assisted surgery deserves your attention. It’s not just a trend—it’s the future of joint replacement.